Can Digital Endpoints Really Accelerate Clinical Trials?
By Anita Burrell, principal, Anita Burrell Consulting LLC
It seems that everything we read today revolves around AI and its potential impacts on the pharmaceutical and biotechnology sector. While generational and agentic AI certainly show promise, the quiet digital revolution is taking place beneath the headlines and hype.
Digital biomarkers are quickly and quietly becoming the digital revolution needed to make clinical trials quicker and more data rich. In this three-part series, discover answers to the following common questions about digital endpoints:
- What are digital endpoints, and why are they trending? Plus, discover the current landscape of how they can be embedded in studies through case examples.
- How has the regulatory environment pathway changed to incorporate digital endpoints, and how has that facilitated sponsor adoption?
- How do companies justify the up-front costs of enabling technology through return on investment analysis?
So, What Are Digital Endpoints?
In traditional clinical trials, endpoints — measurable outcomes such as lab results, imaging studies, and clinical assessments — are usually collected during scheduled visits at the clinic. While some of these may be facilitated by technology at the site, such as ePRO or eCOA, truly digital endpoints are derived from data captured continuously or intermittently through digital health technologies (DHTs), often outside of a clinical setting. These endpoints include data collected by wearable sensors, smartphones, or other connected devices and provide a realistic picture of a patient’s daily health and functioning. For example, a wearable activity tracker can monitor a patient’s gait, step count, or even nocturnal activity, offering a continuous measure of mobility that could be more robust than traditional infrequent assessments.
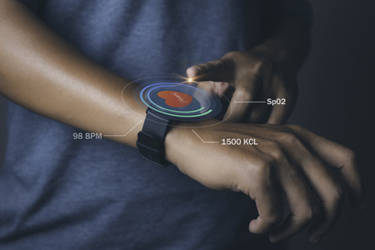
Similarly, digital biomarkers are objective, quantifiable data directly related to biological characteristics collected through digital devices. Digital biomarkers have been implemented to monitor cognitive function in patients with neurodegenerative diseases and track heart rate and blood oxygen levels in real time for clinical trials of Parkinson’s disease, diabetes, and cardiovascular disease.
One of the benefits of digital measures is that they can be collected passively simply by having a participant wear a device (e.g., Apple Watch) that enables the continuous collection of biological characteristics with little burden on the patient. These devices collect real-time health-related information along with context such as the time, place, and measurement conditions, which can enrich the data collection.
Why Are Digital Endpoints A Hot Topic Right Now?
The use of digital endpoints in clinical trials offers several potential advantages. Foremost, digital endpoints provide richer data sets than traditional endpoints (e.g., continuous data collection in a participant’s home environment vs. snapshots/episodic recordings during clinical visits) and perform objective measurements without recall bias, which sometimes flaws patient reported outcomes (PROs), leading to a better understanding of the efficacy and safety of the interventions studied. Digital endpoints can also facilitate decentralized clinical studies via remote data acquisition, potentially increasing diversity and inclusivity in clinical trials while reducing the time to recruit the required trial participants1.
Regulators have recognized their potential, and the first sensor-based DHTs are now included in the FDA’s Medical Devices List2, which includes a focused review of the devices’ overall safety and effectiveness and an evaluation of study appropriateness for the devices’ intended uses and technological characteristics. Examples include continuous glucose monitoring systems and heart rhythm monitors built into the Apple Watch.
Another indicator of their increased acceptance is evidenced by digital endpoints being the subject of proposals for reimbursement for remote patient monitoring in the recent Centers for Medicare and Medicaid Services physical fee schedule3.
And, of course, “Make Health Tech Great Again”4 has propelled the use and acceptance of digital assets further into the American consciousness, including adding an app library at Medicare.gov to highlight trusted, personalized digital health tools focused on prevention, chronic disease management, and cost-effective care navigation.
How Are Digital Endpoints Used In Clinical Trials?
Consider, for instance, the incorporation of a digital endpoint in Bellerophon Therapeutics REBUILD trial in pulmonary fibrosis patients. Bellerophon partnered with ActiGraph to measure participants' physical activity (PA) as the traditional endpoints of oxygen saturation and the 6-minute walk distance. Although that data trended positive, it did not achieve statistical significance in the Phase 2b trial. In the same study, the company incorporated the change in Moderate to Vigorous Physical Activity (MVPA) from baseline as an exploratory endpoint.
According to the case study report5, “the digital endpoint (MVPA) provided the necessary statistical significance and gained FDA endorsement as the sole primary endpoint for Bellerophon's follow-up Phase 3 pivotal trial. The substantial effect size from the Phase 2 data prompted FDA approval to reduce the sample size of the Phase 3 trial from 300 to 140, speeding completion by 18 months and reducing costs. This milestone marked the first time an FDA-endorsed primary endpoint in a pivotal trial was based on wearable data and saved the clinical development program.”
Similarly, we have seen the first acceptance of a digital endpoint for efficacy in clinical trials of Duchenne muscular dystrophy (DMD) by EU regulators6. Functional outcome measures for assessing patients with neuromuscular disease in clinical trials have traditionally consisted of timed tests and motor scales assessed during hospital visits, which can be burdensome to patients with more severe disease and do not capture real-world benefits of therapy. A multistakeholder approach helped develop the stride velocity 95th centile (SV95C), measured by two strap-based sensors worn on the ankles and/or wrists, which has been accepted as an endpoint for DMD drug development programs.7 Finally, a case study in Parkinson’s disease by Merck8 looked at the use of composite digital biomarkers of disease progression to track motor function in a longitudinal clinical study (WATCH-PD), which was anchored to traditional clinical endpoints, such as the MDA-UPDRA Part III. Merck noted that the composite digital biomarker has a >twofold larger progression tracking effect size than MDS-UPDRA Part III, which extrapolated into the need for 73% fewer patients to demonstrate a 20% disease-modifying effect in a one-year trial. Marissa Dockendorf, executive director and head of digital measures at Merck, noted, “Digital health technologies offer tremendous opportunities to quantify the symptoms and progression of Parkinson’s disease with more objectivity, precision, and frequency than traditional clinical rating scales. Our analysis demonstrates that composite digital endpoints hold promise to detect the effects of disease-modifying therapies with significantly smaller trials and to thereby accelerate Parkinson’s disease drug development.”
These case studies illustrate the versatility and granularity that digital endpoints bring to clinical research. By enabling data capture in real-world environments, they not only enhance the sensitivity of outcome measures but also broaden participation to individuals who may be unable or unwilling to travel regularly to study sites.
As digital health technologies continue to evolve — incorporating AI, advanced analytics, and integration with electronic health records — the landscape of what can be measured and how will continue to expand, paving the way for precision medicine and more patient-centered research. In the next article, learn how to ensure regulatory acceptance of digital endpoints in clinical trials and the considerations to ensure successful implementation of these tools.
References:
- The Opportunity of Digital Biomarkers: Unlocking next-generation healthcare, Capgemini 2023 available at https://www.capgemini.com/wp-content/uploads/2024/10/The-opportunity-of-Digital-Biomarkers.pdf
- DiMasi et al, Assessing the net financial benefits of employing digital endpoints in clinical trials, Clin Transi Sci (2024); 17:e13902
- https://www.fda.gov/medical-devices/digital-health-center-excellence/medical-devices-incorporate-sensor-based-digital-health-technology?utm_medium=email&utm_source=govdelivery
- https://natlawreview.com/article/remote-patient-monitoring-rpm-and-remote-therapeutic-monitoring-rtm-what-you-need
- https://www.cms.gov/newsroom/press-releases/white-house-tech-leaders-commit-create-patient-centric-healthcare-ecosystem
- Enhancing clinical insights: De-risking traditional outcome measures in Bellerophon Therapeutics REBUILD study, available at https://datacc.dimesociety.org/resources/enhancing-clinical-insights-de-risking-traditional-outcome-measures-in-bellerophon-therapeutics-rebuild-study/
- Servais et al, Digit Biomark (2021) 5(2): 183-190 available at https://karger.com/dib/article/5/2/183/819698/First-Regulatory-Qualification-of-a-Novel-Digital
- Advancing digital biomarkers to accelerate Parkinson’s disease drug development, available at https://datacc.dimesociety.org/resources/advancing-digital-biomarkers-to-accelerate-parkinsons-disease-drug-development/
About The Author:
 Anita Burrell has over 23 years of pharmaceutical industry leadership experience in the UK, France, and the U.S. in a variety of roles. She led global pricing and reimbursement for Sanofi, directed the development of Aubagio (an oral MS therapy), and was the head of strategic commercial excellence. As the principal of Anita Burrell Consulting LLC since 2015, Anita helps companies understand market dynamics and payer behavior, design integrated evidence plans and value communication projects, as well as understand the implications of digital health and possibilities to use behavioral economics. Anita served on the Healthcare Businesswomen’s Association Global Board of Directors and is the past chair of the ISPOR Digital Health SIG, which addresses opportunities in the healthcare sector emerging from the increasing use of digital technologies. Anita holds a BA (Hons) in economics from the University of Stirling, an MA in economics from Dalhousie University, and an MBA from Kingston University.
Anita Burrell has over 23 years of pharmaceutical industry leadership experience in the UK, France, and the U.S. in a variety of roles. She led global pricing and reimbursement for Sanofi, directed the development of Aubagio (an oral MS therapy), and was the head of strategic commercial excellence. As the principal of Anita Burrell Consulting LLC since 2015, Anita helps companies understand market dynamics and payer behavior, design integrated evidence plans and value communication projects, as well as understand the implications of digital health and possibilities to use behavioral economics. Anita served on the Healthcare Businesswomen’s Association Global Board of Directors and is the past chair of the ISPOR Digital Health SIG, which addresses opportunities in the healthcare sector emerging from the increasing use of digital technologies. Anita holds a BA (Hons) in economics from the University of Stirling, an MA in economics from Dalhousie University, and an MBA from Kingston University.
