Here's A Template — And Tips — For Assessing And Improving Patient Centricity
By Zachary Palazzotto, research engagement intern, and Carol Chapman, MPH, associate director of research engagement, The Crohn’s & Colitis Foundation

Patient centricity has become a buzzword in recent years, and for good reason. Research professionals aim to place the patient at the center of their work, conducting trials that seek to collect complete data sets from diverse groups. To achieve this goal, patient engagement programs have emerged to create and implement practices that integrate patient experiences, perspectives, and priorities into research processes and decision-making. While enthusiasm for patient engagement is high, implementing sustainable programs can be challenging. They require careful planning, commitment, resources, and evaluation. This article provides a guide to review current patient engagement activities and plan for a patient-centric future.
Why You Should Conduct A Patient Centricity Review
Patient centricity can mean many different things. At the Crohn’s & Colitis Foundation, we define it as the meaningful engagement of patients and caregivers and the utilization of their insights throughout all research programs. Functionally, this means we want a diverse group of IBD patients and caregivers to help us set funding priorities, make strategic plans, create recruitment strategies, determine ways to provide value back to study participants, and analyze our data in a manner that is equitable and trusted by the patient community.
The research community recognizes that engaging patients is a priority; however, there is little guidance on creating and maintaining meaningful engagement activities. Whether you are an intern or an associate director, you may feel lost when trying to find a template to measure patient centricity at your organization since few common measures currently exist. To address this unmet need, we created a template to help research departments outline their current patient engagement activities, articulate the impact of these projects, and plan new opportunities that are measurable and sustainable.
Working With A Patient Centricity Review Template
The following information will guide you through each step of the patient centricity program review template. Our approach involves asking questions that will help you communicate various aspects of your program relevant to your success. While this article summarizes each section, here is a link to the template in its entirety: Patient Centricity Program Review. You can reference this document while reading the article.
Setting A High-Level Vision
To avoid getting lost in detail, we began by asking a team to articulate their vision of what an ideal patient engagement program looks like. All subsequent sections should align with this high-level vision. Patient centricity is not about reaching a destination; it is about implementing ongoing practices that continually incorporate the patient perspective. This vision should focus more on aligning activities with patient engagement values and best practices rather than achieving specific goals.
Reviewing Current Patient-Centric Practices
This section defines, classifies, and analyzes current patient engagement activities in your department. The document is designed to be flexible enough to review distinct aspects of research programs. While patient engagement for recruitment may differ from engagement during data analysis, this document allows all aspects of engagement to be included. We also teach you how to classify types of engagement based on the Patient-Centered Outcomes Research Institute (PCORI) Patient Engagement Classification System. Although any form of patient engagement is beneficial, not all engagements are equal. The four main categories are input, consultation, collaboration, and shared leadership. See the image below for a definition of each patient engagement category.
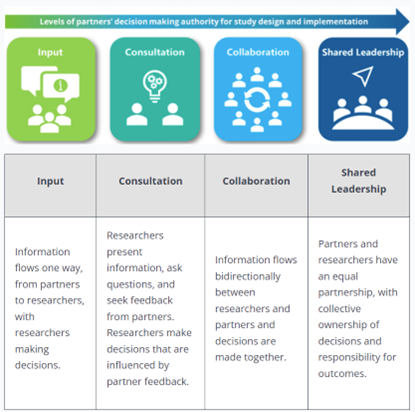
Used with permission from the Patient-Centered Outcomes Research Insitute (PCORI)
In addition to classifying types of engagement, this section reviews communication practices and current obstacles to sustainability. Effective communication significantly influences whether patients feel valued or merely see their involvement as a checkbox exercise. Be honest in this section; without a clear view of current practices, correcting mistakes that could lead to decreased patient engagement becomes challenging.
Securing Support And Resources
Sustainable patient engagement practices require planning, resources, and support from leadership. One major barrier is having adequate resources for effective engagement. In this section, we help identify how patients are educated, informed, and compensated to become effective leaders and advocates. Researchers must assist patients and caregivers in gaining awareness of the research they aim to guide — especially if they were not involved from the outset. Empowering patients involves providing resources such as webinars, learning sessions, and meetings with principal investigators or study teams.
Compensating patients for their time is crucial for building trust and providing value. Budgeting for these activities in advance ensures promises are kept and participants remain engaged. Additionally, accommodating diverse patient populations is essential; some communities may face challenges such as limited internet access or language barriers. Anticipating these needs allows for proper support.
Setting Goals
As previously mentioned, patient centricity is an ongoing network of practices integrating the patient voice into research programs. In this section, we help outline short- and long-term goals for patient engagement and begin developing an action plan to achieve them. Start by identifying each upcoming goal or project while considering staff requirements, workload, project budget, additional tools needed, and necessary approvals.
Identifying Potential Obstacles & Solutions
Identifying obstacles and solutions is essential for addressing unrealistic practices and determining feasible implementation challenges. By describing each challenge related to short- and long-term goals, common denominators across the organization may emerge. Systemic barriers often pose significant limitations; however, anticipating these challenges minimizes uncertainties during implementation. Once obstacles are identified, solutions can be sought before they arise.
Determining What’s Feasible
With an overview of current and future goals, prioritize them based on feasibility regarding workload, budget constraints, obstacle magnitude, and solution practicality.
Planning For Sustainability
After prioritizing goals and selecting projects for advancement, this document will assist in planning for long-term project success. Some activities may only require one-time engagements (e.g., focus groups or surveys), while others — such as advisory committees — demand sustainability planning that includes budgeting and logistical details. Allocating resources ahead of time helps actualize goals effectively.
Choosing Metrics For Monitoring And Evaluation
There is a notable lack of resources for measuring success in patient engagement practices. Identifying key performance indicators (KPIs) is essential for generating impact reports that demonstrate success in these areas. Such reports will facilitate ongoing support for patient engagement initiatives. Although few best practices exist for evaluating engagement efforts, some KPIs used by the Crohn’s & Colitis Foundation include metrics like patient advisory committee attendance rates and annual survey results. Using templates or spreadsheets to track these metrics is crucial for delivering longitudinal results on patient engagement efforts.
Conclusion
Enhancing patient centricity in research necessitates a systematic approach that prioritizes communication outcomes and amplifies patient voices. By continuously evaluating and refining engagement practices, researchers can ensure studies respond effectively to patients’ needs — leading to improved satisfaction and health outcomes while reducing healthcare inequities. Tools like the Patient Centricity Program Review Template facilitate the integration of patient-centric practices into healthcare research frameworks.
About The Authors:
 Zachary Palazzotto is a third-year undergraduate student pursuing a degree in biomedical engineering and public health at the University of Virginia. He was the research engagement intern at The Crohn’s & Colitis Foundation during the summer of 2024 and continued a remote internship into the fall 2024 semester at the Foundation. Zachary worked with an array of study teams to review their patient-centric practices with the goal of developing the Patient Centricity Program Review. At the University of Virginia, Zachary is a three-time elected member of the Engineering Student Council, gives weekly tours of the engineering school, volunteers in the Albemarle County School District, and builds low-cost microscopes in his research laboratory. After graduating in May 2026, he plans to begin his career in the clinical trial operations field where he hopes to design diverse and equitable research studies, ensuring patient voices are included every step of the way.
Zachary Palazzotto is a third-year undergraduate student pursuing a degree in biomedical engineering and public health at the University of Virginia. He was the research engagement intern at The Crohn’s & Colitis Foundation during the summer of 2024 and continued a remote internship into the fall 2024 semester at the Foundation. Zachary worked with an array of study teams to review their patient-centric practices with the goal of developing the Patient Centricity Program Review. At the University of Virginia, Zachary is a three-time elected member of the Engineering Student Council, gives weekly tours of the engineering school, volunteers in the Albemarle County School District, and builds low-cost microscopes in his research laboratory. After graduating in May 2026, he plans to begin his career in the clinical trial operations field where he hopes to design diverse and equitable research studies, ensuring patient voices are included every step of the way.
 Carol Chapman, MPH is the associate director of research engagement at The Crohn’s & Colitis Foundation. She uses her background in clinical research coordination and public health to develop and implement new ways to engage patients in all research activities. She works to include diverse patient voices as experienced leaders who can help research teams provide more value to their participants. By engaging patients early and often throughout the research process, she aims to build trust, improve recruitment practices, and increase adherence to study activities. Before joining the Foundation, Carol worked in the hospital, community, and digital health technology sectors where her work focused on patient recruitment, diversity in research, and building trust in groups historically harmed by medical research.
Carol Chapman, MPH is the associate director of research engagement at The Crohn’s & Colitis Foundation. She uses her background in clinical research coordination and public health to develop and implement new ways to engage patients in all research activities. She works to include diverse patient voices as experienced leaders who can help research teams provide more value to their participants. By engaging patients early and often throughout the research process, she aims to build trust, improve recruitment practices, and increase adherence to study activities. Before joining the Foundation, Carol worked in the hospital, community, and digital health technology sectors where her work focused on patient recruitment, diversity in research, and building trust in groups historically harmed by medical research.
