Hey, What's The Big Idea? Patient Enrollment Utterly Reimagined, That's What
By Tatty Scott, patient engagement and recruitment professional

Whatever we throw at the problem of patient enrollment, nothing seems to move us reliably away from our 80% failure rate.1 It’s time we adopted the proven performance methods of high reliability organizations (HROs). While radical, it’s a necessary reform.
What If Air Traffic Control Failed 80% Of The Time?
HROs include air traffic control, nuclear power plants, and aircraft carriers. They are organizations that operate in high-risk environments and should have a high accident rate but do not. When they do fail, because procedures haven’t been followed, the results are catastrophic and make front page news.
High reliability theory, based on studies of these organizations, emerged in the 1980s as a response to Charles Perrow’s normal accident theory, 2 which asserts that, “Whatever you do, shizz happens.” I paraphrase.
In 1989, researcher Karlene Roberts queried why normal accident theory didn’t hold water in high-risk industries such as nuclear power and naval aircraft carriers. She coined the term high reliability organizations to describe these normal-accident anomalies.3
Jump forward a decade, and researchers Karl Weick and Kathleen Sutcliffe had further developed the concept, redefining reliability as performance and identifying five key principles that all HROs live by: 4
- Preoccupation with failure
- Reluctance to simplify
- Sensitivity to operations
- Commitment to resilience
- Deference to expertise
As you can probably deduce, in high-reliability settings, nothing is left to chance. If a dial is even a millimeter off its mark, there’s no wait-and-see, there’s no blame game, and it’s definitely not left until David gets back from PTO.
Since publication of the work of Roberts, Weick, and Sutcliffe, HRO principles have been adopted by industries as diverse as healthcare, construction, and education. But based on a literature review, they have not been adopted in clinical trials to tackle our patient enrollment stasis. Yet.
A Lousy Girlfriend, But A Great Patient Recruitment Fixer
Put simply, clinical trials exist to get the best drugs to patients. To achieve this, our key objective is to enroll enough patients to demonstrate safety and efficacy. But getting to the point of enrollment is quite the convoluted baton race.
When we look at the patient enrollment ecosystem and honestly assess the motivations and behaviors of all the different stakeholders involved throughout the journey — sites, vendors, CROs, patients, sponsors — we see disparate challenges, pain points, and objectives. From personal experience, even different teams within the same organization can be operating in silos and not pulling together, not even communicating.
My role in the system has been patient engagement, recruitment, and retention. Based on my experiences, too often, by the time we’re handed the baton and asked to devise a patient recruitment strategy, the final protocol and feasibility report are a done deal with little to no input from patient recruitment experts. Low patient recruitment, so often cited as the main reason for enrollment failure5,6, isn’t a patient recruitment failure per se. It is just that what is handed to our teams isn’t deliverable, like being given three pots of emulsion to paint the ceiling of the Sistine Chapel. By Friday. I know through conversations that many stakeholders in different areas of the ecosystem feel the same way.
Now, as a worrier with an innate need to fix things, I make a lousy girlfriend to be fair. But discovering high-reliability principles and mapping them against my frustrations at work has given my neuroses wings. Here are a set of five proven operating principles that when applied systemically can fix patient enrollment.
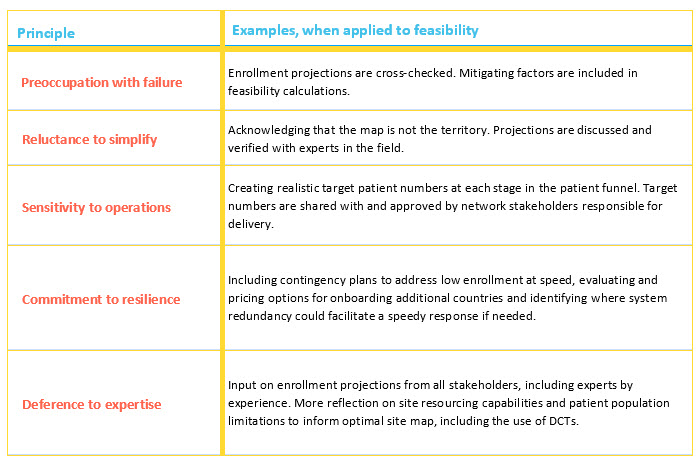
For instance, let’s start with a basic first pass at applying the principles to feasibility. (I’m picking feasibility because Briel7 found 28 different reasons for recruitment failure; the most frequently reported was “overestimation of the prevalence of eligible patients.”)
How might the five principles shape feasibility to correct this overestimation?
The Reality (Cost And Buy-In Included) Of Adopting HRPs
As a worrier, I am now thinking that you’re thinking, “Well, this is all very well in theory but what is the actual road map from a standing start to wholesale adoption of HRPs? I’ll wait.”
I’m more than happy to meet to chew over how this will work. For now, though, let me start by addressing three core elements as I see them.
1. How Will HRPs Work In Practice?
- What’s imperative in an HRO is that all team members coalesce around joint objectives. For us in clinical trials, our core objective is to reach patient enrollment. A fundamental change, therefore, is that all stakeholders’ KPIs will include their explicit contribution to the joint objective of achieving patient enrollment. And yes, that also means those writing the protocol have to show how it will explicitly support patient enrollment.
- To optimize HRPs’ impact on enrollment performance, they need to be applied across every element of the system. In Russ Ackoff’s talk on quality and improvement programs using systems thinking, he states that “If we have a system of improvement that is directed at the parts taken separately, you can be absolutely sure that the performance as a whole will not be improved… The reason for the failures [of quality and improvement programs] is primarily the fact that they have not been embedded in systems thinking. They have been anti-systemic applications.”8 In other words, we can’t improve patient recruitment without also looking at where it fits within our system. Ackoff uses the analogy of a car to demonstrate how all parts within a system are interdependent. Our interdependence, however, isn’t mechanical. We need to think of our system as an orchestra, with different sections working together to reach our shared objectives under the guidance of a conductor (HRPs).
- This new HRP model requires a root and branch change in how we do things. Silos, buck-passing, and billable hours that do not directly improve patient enrollment are out, replaced by a focus on solutions. All of us within the ecosystem become part of a mycorrhizal network — like fungi communicating throughout a forest — a communicative feedback web, sensitive at all times to any movement within patient enrollment. If/when the enrollment needle drops a millimeter from where it should be, the network knows and responds.
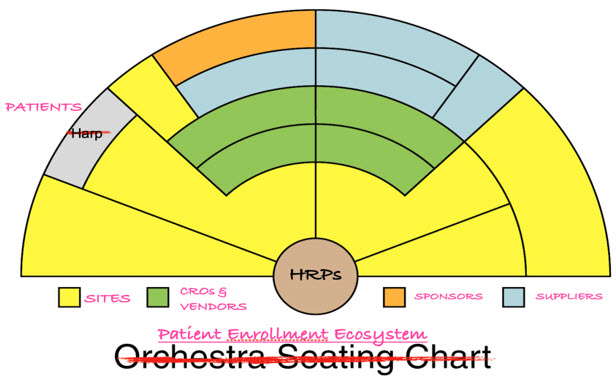
A standard orchestra seating chart adapted to reflect systems thinking for our patient enrollment ecosystem. As I have no graphic design skills whatsoever, I accessed this free download from abcteach.com with thanks.
2. How Much Will It Cost?
- It is important to start by saying that the value of a single day of clinical trial delay is around $540,0009. Every. Single. Day. That’s an eye-watering $16+ million a month, and clinical trial delays can exceed 12 months10. Ouch.
- There will be costs to improve effectiveness, but there will also be savings. In applying HRPs, we’re going to be doing things we are already doing — feasibility, site selection, patient engagement — but we’re going to be doing them better and more rigorously.
- Certainly, our conversations will be different, starting more often with “What’s not working, and how do we fix that?” (So maybe factor in time costs for editing SOPs? I am being facetious, but only slightly.) An additional cost will be the salary of an HRP architect/conductor to embed the principles into the system and coordinate the orchestra.
- The bottom line is, through their fundamental purpose of delivering reliability and performance, HRPs qualify the investment of up-front spend; additional costs in improving responsiveness and effectiveness will be light years away from our current extension losses.
3. What About Workforce Resistance?
- Do I really think all these enrollment stakeholders are going to go for the roots and branches and mushrooms? Yes, I do. You see, since the 1950s, (good) human resource management has been moving away from the command-and-control approach so beloved by autocrats. The current thinking is that the best motivators at work include achievement and responsibility11, as well as autonomy, mastery, and purpose.12
- In John Purcell’s seminal Unlocking the Black Box: Understanding the People and Performance Link,13 researchers explored the impact of AMO policies on performance — how people perform well when they have the ability (skills), the motivation, and the opportunity. Importantly, the opportunity element is not simply a chance to deploy their skills but to use them to contribute to their work groups and organizational success.
- In addition, Purcell and team found that a “big idea” within a business improved performance. The idea becomes “a collective endeavor or a sort of glue binding people and processes together.” They concluded that the big idea can provide a means of measuring performance and an opportunity to integrate different business functions.
- In our high-reliability model, the mycorrhizal network allows each stakeholder to apply their skills to support the study’s enrollment success. Achieving patient enrollment on time through the HRP prism is the big idea that binds people and processes together.
Radical Reform
I’ve learned a lot of things over the years. I’ve learned you should never drive a tractor with your mouth open. I’ve learned that it’s inadvisable to pluck your eyebrows when you’re in a hurry. And I’ve learned that our patient enrollment system is broken.
But, on a positive note, I have learned that high-reliability principles work. Weick and Sutcliffe, with their organizational chops, have shown that the application of high-reliability principles leads to high-performing organizations.
So, let’s become high-performing; nothing is stopping us but ourselves. Let’s take this proven methodology and apply it, not at the point of writing a patient recruitment strategy but systemically from the first page of the score and for our entire orchestra.
We do what we do to get the best drugs to patients faster. I propose that applying high-reliability principles is the optimal route.
References:
- Desai, M. Recruitment and retention of participants in clinical studies: Critical issues and challenges. Perspectives in Clinical Research. 2020;11(2), pp51-53
- Perrow, C. Normal Accidents: Living with High-Risk Technologies. Basic Books, New York. 1984
- Roberts, K. H. New challenges in organizational research: high reliability organizations. Industrial Crisis Quarterly. 1989;3(2), pp111–125
- Weick, K. E., & Sutcliffe, K. M. Managing the unexpected: Assuring high performance in an age of complexity. Jossey-Bass. 2001
- Briel, M. et al. Exploring reasons for recruitment failure in clinical trials: a qualitative study with clinical trial stakeholders in Switzerland, Germany, and Canada. Current Controlled Trials in Cardiovascular Medicine. 2021;22 (1), 844–844
- Bose, D. et al. Fstakeholders influencing recruitment and retention of participants in clinical studies conducted at a tertiary referral center: A five-year audit. Perspectives in clinical research. 2020;11 (2), 81–85
- Briel M, Olu KK, von Elm E, Kasenda B, Alturki R, Agarwal A, et al. A systematic review of discontinued trials suggested that most reasons for recruitment failure were preventable. J Clin Epidemiol. 2016;80:8–15.
- Ackoff, R. 1994; Recorded Presentation on Systems Thinking and Quality Improvement; Accessed June 11 2025.
- Getz, K. 2024, Available at: https://www.appliedclinicaltrialsonline.com/view/how-much-does-a-day-of-delay-in-a-clinical trial-really-cost- Accessed 27 Jan 2025
- Shadbolt C, Naufal E, Bunzli S, et al. 2023; Analysis of Rates of Completion, Delays, and Participant Recruitment in Randomized Clinical Trials in Surgery. JAMA Netw Open;6(1):e2250996. doi:10.1001/jamanetworkopen.2022.50996.
- Herzberg, F., Mausner, B. and Snyderman, B. The Motivation to Work. 2nd Edition, John Wiley & Sons Inc., New York. 1959; 20, 141-147
- Pink, Daniel H.. Drive: The Surprising Truth About What Motivates Us. Riverhead Books, New York. 2011.
- Purcell, J., Kinnie, N., Hutchinson, S., Rayton, B., Swart, J. Understanding the People and Performance Link: Unlocking the Black Box, CIPD, London. 2003.
About The Author:
 Tatty Scott is a patient engagement and recruitment professional based in Scotland. She worked as a journalist, focusing on health, and in diverse community engagement for 20 years before joining clinical trial engagement in 2015. Her favorite food is oranges, and she has a cocker spaniel named Piglet.
Tatty Scott is a patient engagement and recruitment professional based in Scotland. She worked as a journalist, focusing on health, and in diverse community engagement for 20 years before joining clinical trial engagement in 2015. Her favorite food is oranges, and she has a cocker spaniel named Piglet.
