Making Medical Innovation Matter To Patients With Simplified Trial Design
By Craig Granowitz, MD, Ph.D., chief medical officer, Lexicon Pharmaceuticals
Translating breakthrough science into real-world patient benefit is the ultimate aim of the biopharma industry. In our love of science, we can potentially lose sight of the fact that medicines must not only demonstrate efficacy and safety but also be in tune with how patients live their lives.
Regulatory agencies worldwide are encouraging biopharma sponsors to adopt more flexible, patient-centric approaches to clinical research, while maintaining rigorous standards for safety and efficacy. This evolving environment presents both opportunities and challenges for clinical, regulatory, and compliance professionals across the industry.
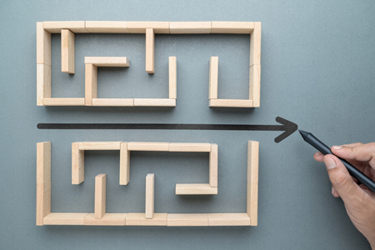
To be a leader in today’s environment, companies must embrace pragmatic innovation — an approach embedded naturally in simplified clinical trial designs, which can reduce regulatory risks, lower R&D costs, and shorten clinical timelines — all for the benefit of patients. Crucial to addressing the challenges associated with complex, traditional trials, pragmatic innovation can not only help streamline trial operations but also lead to faster answers for patients in need.
Balancing Speed And Rigor In Regulatory Processes
With growing demand for timely access to innovative therapies, both sponsor companies and regulators are rethinking how to streamline drug development and approval processes.
Regulatory agencies, including the FDA and the EMA, are increasingly open to novel trial designs and the use of real-world evidence (RWE) and patient-reported outcomes (PROs) in applications, especially for diseases that have critical treatment needs. At the same time, sponsors are engaging regulators earlier, more frequently, and with greater transparency to align on trial endpoints, patient populations, and overall evidence requirements.
Consider the example of data packages required for an NDA. Rather than requiring the sponsor to generate all evidence through its own trials, a willingness by regulatory agencies to review and accept data from investigator‑initiated studies could save years and potentially millions of dollars. These studies often use simplified designs that better reflect real‑world practice and focus on endpoints aligned with what patients actually experience. Leveraging such studies could streamline data generation and complexity while adhering to core efficacy, safety, and quality principles.
Reducing Costs Without Compromise
Speed and efficiency are particularly important in the current financial climate, where the cost of capital is high, funding windows are short and unpredictable, and companies must be both strategic and nimble about how they invest their resources and de-risk their clinical programs. Through simplified clinical trial designs, companies can significantly decrease the financial burden associated with traditional, more complex trials, while accelerating timelines for value creation and funding milestones. Cost reduction does not mean cutting resources but optimizing them to ensure that every dollar contributes directly to the development of effective therapies and then constantly reevaluating additional program funding commitments.
Using Lexicon Pharmaceuticals as an example, we have recently employed AI analysis of a large patient data set comprising multiple Phase 2 studies to test and validate assumptions about baseline patient characteristics. We believe these assumptions will enhance the probability of Phase 3 success by mitigating potential placebo effects in the study control group. This not only reduces costs but also increases the likelihood of successful outcomes for us and patients.
Shortening Timelines To Accelerate Development
A more pragmatic approach can also support shortened timelines of therapeutic development, help to consolidate various phases, focus on key outcomes, and minimize redundancies. Instead of proceeding with a trial sequentially, companies are increasingly embracing strategies that allow simultaneous exploration of different facets of a treatment and, in turn, reduce overall time to market. This “in parallel” approach must always be balanced against increased resource burn. Balancing time and risk can be aided by increasing the frequency of clinical trial milestones and seeking alternative funding sources and partnerships.
Case In Point: Evolving Trial Designs For Hypertrophic Cardiomyopathy
Putting pragmatic innovation into action is particularly clear in how we at Lexicon have structured our clinical development program for sotagliflozin in hypertrophic cardiomyopathy (HCM), including the design of our ongoing Phase 3 SONATA-HCM study. HCM is a genetic cardiac disease that causes the heart muscle to thicken, making it difficult to pump blood. Over the last decade, researchers and clinicians have made significant advancements in understanding the underlying mechanisms of HCM and diagnosing the condition, and several biopharma companies have initiated development of new investigational treatments. However, the clinical studies traditionally used to evaluate the efficacy and safety of HCM therapies are typically time-consuming and costly. Therefore, we asked ourselves: How can we combine our genetic and cardiometabolic expertise with a pragmatic approach to clinical trials to bring an HCM treatment to patients quickly, with lower risk, and at a lower cost?
Typically, companies run separate sequential studies for obstructive and non-obstructive HCM. In contrast, based on our experience in heart failure and related conditions, we developed a medical and scientific rationale for a streamlined and relatively de-risked program in HCM with sotaglifozin . Due to established academic relationships, an evolving understanding of the genetic and metabolic basis of HCM pathophysiology, and previous regulatory interactions, we developed a program consisting of a single pivotal study enrolling both obstructive and non-obstructive patient populations in a single registrational study — our randomized, double-blind, placebo-controlled, multicenter SONATA-HCM trial. This program design dramatically reduced program timelines and costs. The simplified trial design also prioritized KCCQ (a patient-reported outcome metric) as the study’s primary endpoint, which further simplified the trial design and increased the universe of potential study sites.
Currently, SONATA-HCM is enrolling participants in 130 study sites in 20 countries. If the results are positive, we expect the study to support a broad label for sotagliflozin, which is already approved for heart failure, to treat both obstructive and non-obstructive HCM.
As regulatory agencies continue to encourage flexible, efficient approaches, regulatory professionals are in an ideal position to drive these changes. By focusing on efficiency, patient experience, and regulatory collaboration, and sharing best practices and lessons learned with the industry, biopharma professionals can collectively set new standards and accelerate the delivery of life-changing medicines to patients.
About The Author:
 Craig B. Granowitz, MD, Ph.D., has been the senior vice president and chief medical officer at Lexicon Pharmaceuticals since August 2021. Before that, Dr. Granowitz served as chief medical officer of Amarin Corporation plc. Prior to joining Amarin, he served as senior vice president and head of global medical affairs, global human health of Merck & Co., Inc. and in various medical and commercial management positions for Schering-Plough Corporation. Dr. Granowitz received a B.A. from Dartmouth College and an MD and Ph.D. from Columbia University.
Craig B. Granowitz, MD, Ph.D., has been the senior vice president and chief medical officer at Lexicon Pharmaceuticals since August 2021. Before that, Dr. Granowitz served as chief medical officer of Amarin Corporation plc. Prior to joining Amarin, he served as senior vice president and head of global medical affairs, global human health of Merck & Co., Inc. and in various medical and commercial management positions for Schering-Plough Corporation. Dr. Granowitz received a B.A. from Dartmouth College and an MD and Ph.D. from Columbia University.
