Precise Patient Recruitment Planning – It's All About The Patient Pathway
By Beth Harper
 At this stage in my career, I confess that I’ve lost track of the number of publications and presentations I’ve developed and delivered on the topic of patient recruitment. Many of these have focused on lessons learned from troubleshooting hundreds of trials in “rescue mode.” As I reflect on why so many recruitment campaigns or efforts fail to deliver the expected results, a common root cause issue points to the lack of understanding of the importance of, and how to create, a meaningful patient pathway. This terminology may mean different things to different individuals and organizations and may be used interchangeably with patient journeys.
At this stage in my career, I confess that I’ve lost track of the number of publications and presentations I’ve developed and delivered on the topic of patient recruitment. Many of these have focused on lessons learned from troubleshooting hundreds of trials in “rescue mode.” As I reflect on why so many recruitment campaigns or efforts fail to deliver the expected results, a common root cause issue points to the lack of understanding of the importance of, and how to create, a meaningful patient pathway. This terminology may mean different things to different individuals and organizations and may be used interchangeably with patient journeys.
For the purposes of this discussion, I use the term patient pathway to mean a visual representation of how a patient (prospective research subject) navigates through the healthcare system and the touch points where they might learn about and encounter opportunities to get involved in a given clinical trial. So why is this the key to precision when it comes to planning patient recruitment efforts? Because without this, study teams and sites aren’t able to systematically identify the most strategic or “high yield” sources of subjects and the best tactics to ensure these sources are aware of the study opportunity. This results in a shotgun approach to the deployment of recruitment campaigns, wasted time and effort, and, ultimately, very poor returns on the recruitment enhancement investments.1
The Patient Pathway Development Process
The process, which can be done by anyone involved with patient recruitment at the site, sponsor, CRO, or vendor level, is to start answering the questions in Figure 1.
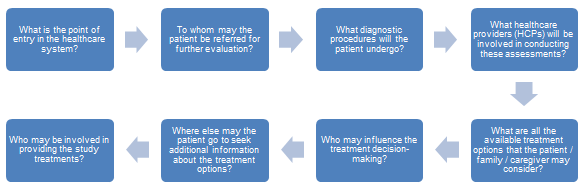
Figure 1
A generic set of responses can be crafted to start an illustrative or representative pathway (i.e., start with the U.S. healthcare system), recognizing that this will need to be adapted to reflect the nuances and differences across regional and country-specific healthcare systems.
The next step is to translate this into some type of visual road map so that all parties involved in planning the recruitment and study awareness campaign can visualize the flow of the patient from entry into the healthcare system to the point of arrival into the clinical trial. This can take various forms (see below), but from the visual map it becomes easier to identify the following key information:\
- Who are the primary HCPs that are most likely in a position to be a source of subjects (identifying and referring them and/or providing them information about the trial opportunities)?
- Where are all of the places, venues, and times the patient might be able to learn about the trial opportunities?
Answering these key questions naturally leads to the ability of the recruitment strategy planners to link the tactics for study awareness building and education to the potential sources. From there, the relevant materials can be developed and the potential resources needed to support the recruitment tactics secured as noted in Figure 2.
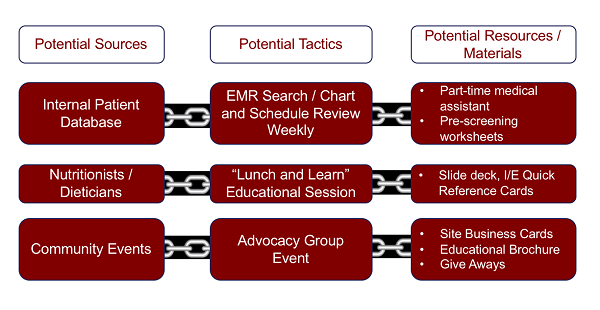
Figure 2
Visual Pathways — Examples And Value
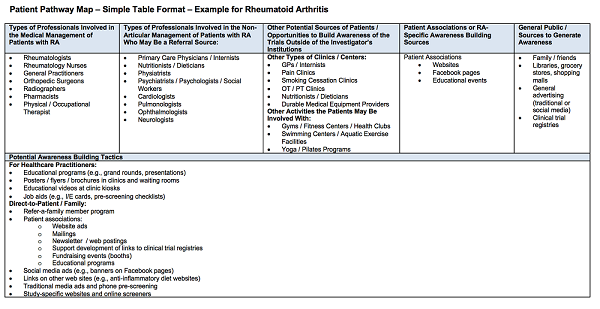
From the simple exercise above, there are a number of ways that the patient pathway can be mapped to link sources of patients to awareness-building opportunities and venues to materials. This can take the form of a simple table, as shown in Figure 3.
Figure 3
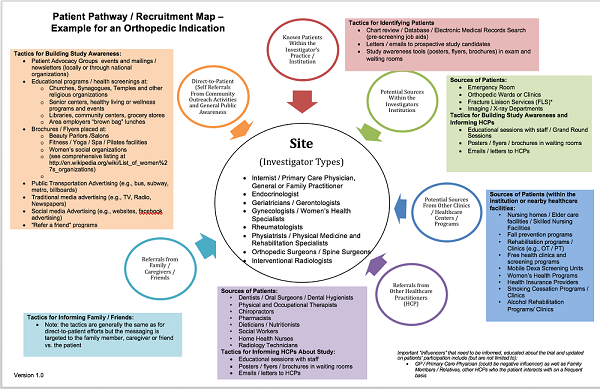
Or they could take the form of a variety of visual maps, ranging from relatively simple (Figure 4)…
Figure 4
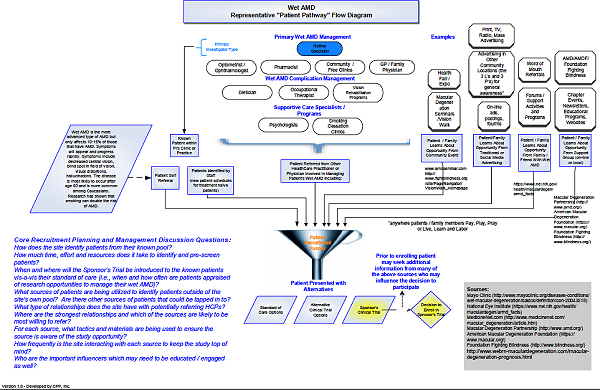
… to more complex (Figure 5).
Figure 5
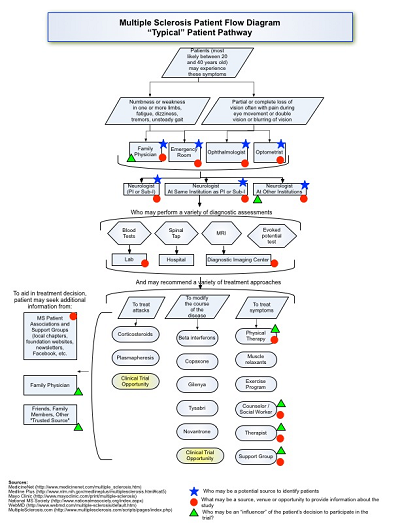
They could even include process flow types of pathway illustrations, as shown in Figure 6.
Figure 6
There is no one right way to do the mapping, but the value comes in using these maps as communication tools to help in the recruitment planning process. Instead of going for the default “let’s do a social media campaign,” team members can walk through the maps to determine if there are other venues or forums for building awareness that could be more impactful. From the Center for Information and Study on Clinical Research Participation’s research, we know that most participants start their search for clinical trial opportunities with their primary care providers/physicians — and prefer to do it that way.2
Walking through the visual maps may reveal which types of HCPs “touch” the patient earlier in the treatment and evaluation process. Targeting these sources with educational materials and a mechanism to refer patients may represent a more target-rich environment to focus on than casting wider nets through media campaigns. This can be critically important when it’s important to “catch” a potential subject before they are exposed to a particular treatment, if such treatment would exclude a subject from participating. This may be a nuance that is lost when targeting subjects through other public awareness campaigns.
Further, color-coding the maps to identify important influencers of the participant’s decision-making process may uncover other missed opportunities for who is important to reach and/or keep informed, as these could play an important role in the subject’s willingness to participate in the trial. As all of these examples illustrate, there are ultimately a variety of sources, tactics, and materials that can be implemented, but this process helps team members to prioritize those opportunities that will be more impactful.
Patient Pathway Validation And Implementation
From the generic or representative pathway, it’s important to validate the findings with study sites and local country representatives. As the saying goes “one size does not fit all” in patient recruitment, and what will work for one country, region, site, or type of site will not work for others. Having the visual map as a prop during feasibility and site selection discussions can be very enlightening. Teams may find that treatment options that are available in one region are not available in others or that all subjects go to a specialty type of healthcare center for diagnosis and treatment versus a more distributed model. Noting the important differences allows the recruitment strategy planners to customize their approaches to accommodate these differences rather than foisting materials and tools upon sites only to find they aren’t a cultural, ethical, or even logistical fit.
Finally, these visual maps serve as a great resource once recruitment is underway. If the site has exhausted its known pool of patients and requires additional efforts to build study awareness, the patient pathway can be a valuable resource. By using the maps, sites may discover there are some nontraditional types of HCPs further upstream in the diagnosis and treatment pathway that they may not have thought of. Targeting these specific sources in more strategic ways beyond a generic “Dear Doctor” letter may prove very effective.
As the saying goes, a picture is worth a thousand words. Patient pathways, as described here, offer a great picture of the process for how, when, and where a patient may flow into a clinical trial and provide a means of increasing the precision and predictability of recruitment planning efforts.
References:
- https://www.clinicalleader.com/doc/do-patient-recruitment-advertising-awareness-campaigns-really-work-0001
- CISCRP 2017 Perceptions & Insights Study – Report on The Participation Decision-Making Process.
About The Author:
 Beth Harper is the president of Clinical Performance Partners, Inc., a clinical research consulting firm specializing in enrollment and site performance management. She also is the workforce innovation officer for the Association of Clinical Research Professionals (ACRP). Harper has passionately pursued solutions for optimizing clinical trials and educating clinical research professionals for over three decades. She is an adjunct assistant professor at George Washington University who has published and presented extensively in the areas of protocol optimization, study feasibility, site selection, patient recruitment, and sponsor-site relationship management. She serves on the CISCRP Advisory Board and the Clinical Leader Editorial Advisory Board, among other industry volunteer activities.
Beth Harper is the president of Clinical Performance Partners, Inc., a clinical research consulting firm specializing in enrollment and site performance management. She also is the workforce innovation officer for the Association of Clinical Research Professionals (ACRP). Harper has passionately pursued solutions for optimizing clinical trials and educating clinical research professionals for over three decades. She is an adjunct assistant professor at George Washington University who has published and presented extensively in the areas of protocol optimization, study feasibility, site selection, patient recruitment, and sponsor-site relationship management. She serves on the CISCRP Advisory Board and the Clinical Leader Editorial Advisory Board, among other industry volunteer activities.
Harper received her B.S. in occupational therapy from the University of Wisconsin and an M.B.A. from the University of Texas. She can be reached at 817-946-4728, bharper@clinicalperformancepartners.com, or bharper@acrpnet.org.