The Clinical Trials Transformation Initiative: Shaping The Future Of Clinical Research
By Sally Okun, Clinical Trials Transformation Initiative
The time to create true and lasting change in clinical trials is now and the Clinical Trials Transformation Initiative (CTTI), a group of individuals and organizations that want to improve the quality and efficiency of clinical trials, is working to shape a future of smarter, faster, more inclusive clinical research. Co-founded by Duke University and the U.S. Food and Drug Administration (FDA) in 2007, CTTI identifies and addresses challenges to well-designed, properly executed clinical trials and creates actionable recommendations to improve clinical trials and modernize research.
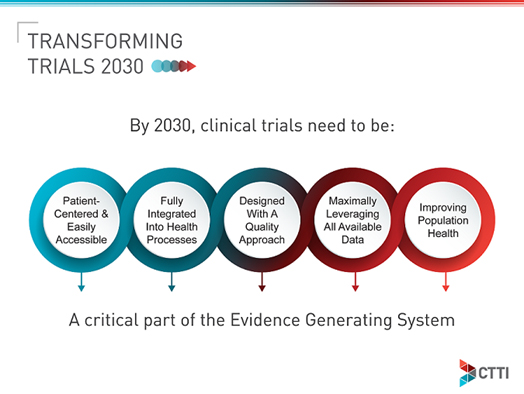
Earlier this year, the CTTI community launched a vision for how clinical trials should be done in 2030. Our vision, Transforming Trials 2030, is one that all stakeholders can aspire to achieve together. The aim of the five-part vision is to build a new generation of clinical trials that more aptly benefit research, healthcare, and — most importantly — people.
To achieve this vision, CTTI is building on its long history of bringing together all stakeholders — 500+ organizations and approximately 80 member organizations — from across the clinical trials ecosystem to discuss issues, exchange ideas, and come to a consensus on solutions. Together, these diverse organizations and individuals work on the most important and forward-looking issues in clinical research — those that will generate high-quality evidence faster and, ultimately, improve the health of people.
We recognize that cross-system collaboration will be critical to unlocking the changes needed to make Transforming Trials 2030 a reality. The full Transforming Trials 2030 vision is that by 2030:
1. Clinical trials are patient-centered and easily accessible.
- Patients and patient organizations are fully integrated in the design and governance of clinical trials, helping to ensure the relevance of the research questions and completeness of outcomes.
- When possible, individuals are involved in clinical trials without going to designated clinical sites to enroll or participate.
- Home trials, hybrid trials, and technologies are maximally used to allow all potential participants to take part regardless of geography and mobility and to maximize efficiency and minimize costs.
- Every potential participant is aware of clinical trials relevant to them.
- Enrolled clinical trial participants reflect the diversity of the population expected to use the medical product.
2. Clinical trials are fully integrated into health processes.
- Trials are integrated within learning healthcare systems where science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by-product of the delivery experience.
- Clinical trial data are collected via the electronic health record (EHR), with additional data collected only if unavailable in the EHR.
- Informed consent for clinical trial participation is integrated into the care process. Consent policies are directly tied to risk mitigation in a clinical study and are easily understood by trial participants.
- Healthcare systems and health plans are involved in planning studies and support the integration of trials into regular clinical practice in order to facilitate engagement of care providers, recruitment, data collection from EHRs, and uptake of trial results.
3. Clinical trials are designed with a quality approach.
- Clinical trials address clear and meaningful scientific questions that are determined with the input and consideration of those who will use the results, including care providers, regulators, and payers.
- Clinical trials are fit for purpose, designed with study activities that are essential to ensure the safety of trial participants and the credibility of key study results and with nonessential activities eliminated to simplify conduct, improve trial efficiency, and target resources to most critical areas.
- A broad range of relevant stakeholders, internal and external to the sponsor organization (e.g., patients and study coordinators), are involved in protocol development and discussions around study quality of individual trials.
- Consideration is given to the validity and efficiency of clinical trials prior to their conduct, including the clarity and conciseness of the protocols and informed consent materials, the ease of adequate data collection that is not excessive, and the validity of analysis plans matched for the purposes of the trials.
- Innovative trial designs (e.g., statistical approaches) will continue to be developed and used to more efficiently and effectively conduct clinical trials.
- Where possible, clinical trial infrastructure is reused.
4. Clinical trials maximally leverage available clinical and nonclinical data, including data collected via digital technologies, to minimize collection of necessary trial specific data.
- Clinical trials are enhanced by the integration of new types of data, such as consumer and digital data.
- Data are accessible, with appropriate governance and controls, to all researchers and sponsors.
- Use of EHR data and other relevant available data from trial participants is straightforward.
- Linkage with health plan claims data for trial participants is simple when beneficial for trial conduct.
- Data platforms support multiple clinical trials, rather than being built for individual trials.
- Choices of data sources and methodologies correspond to the level of evidence needed to answer the research question and consider how the study results will be used.
- Data standards and definitions are in place to support integration of data from various sources, and the systems are interoperable.
- Common standards exist to address privacy and security in an easily implementable and transparent manner.
5. Clinical trials contribute knowledge about how to prevent, diagnose, and treat disease, and clinical trials are one of many sources of information that can be acted upon to improve population health.
- New medical products are available to care providers and patients more quickly and efficiently than today.
- Results of trials are broadly shared with participants and care providers, so they can be considered as part of the totality of evidence and acted upon for the benefit of the public’s health.
- With less expensive and more efficient clinical trials, more clinical trials and other types of research are done to answer the questions most important to patients.
Each pillar of Transforming Trials 2030 reflects CTTI’s core values that are foundational to the organization’s work. While most of CTTI’s projects and activities focus on clinical trials involving FDA-regulated medical products and procedures, we are also part of the global clinical trial community and frequently engage with colleagues around the world as opportunities arise.
As CTTI’s new executive director, I look forward to embarking on this transformative journey guided by the values that have served CTTI and the clinical trials community well since 2007:
- Acting in the interest of the public’s health to improve clinical trials
- Making publicly available recommendations and resources to improve clinical trials
- Holding paramount the need to protect trial participants
- Ensuring quality of clinical trial data is appropriate for decision-making needs
- Valuing the input and participation of all stakeholders equally
- Identifying and managing conflict of interest and bias
- Ensuring integrity and transparency of CTTI activities
Reaching these goals for the benefit of patients is only going to work if each and every one of us moves forward in our respective areas of challenging and advancing clinical research. And there has never been a better time to push thinking, challenge assumptions, and create improvements across the complex clinical trials ecosystem. CTTI is excited about the impact we can have when we work together with the clinical trials community.
We welcome others to join us — add your name and commitment to our growing list of supporters; communicate the vision with colleagues and your followers on social media; access and share our full Transforming Trials 2030 document; and reach out to the CTTI team to learn more about how you or your organization can join in making this vision a reality.
About The Author:
 Sally Okun is the executive director of the Clinical Trials Transformation Initiative (CTTI). She provides senior oversight and management of CTTI operations and organizes efforts to leverage the participation of member organizations and external stakeholders. Prior to joining CTTI, Okun most recently served as the vice president for policy & ethics at PatientsLikeMe. While there, she led a newly established ethics and compliance advisory board. A registered nurse, Okun previously practiced as a palliative and end-of-life care specialist for nearly three decades and contributed to multiple clinical, research, and educational projects in that specialty area.
Sally Okun is the executive director of the Clinical Trials Transformation Initiative (CTTI). She provides senior oversight and management of CTTI operations and organizes efforts to leverage the participation of member organizations and external stakeholders. Prior to joining CTTI, Okun most recently served as the vice president for policy & ethics at PatientsLikeMe. While there, she led a newly established ethics and compliance advisory board. A registered nurse, Okun previously practiced as a palliative and end-of-life care specialist for nearly three decades and contributed to multiple clinical, research, and educational projects in that specialty area.
