6 Tips To Ensure Revenue Integrity And Compliance In Clinical Operations
By Sachit Verma, MD, MBA, FACHE, FAPCR

Revenue integrity and compliance are essential in clinical research operations for financial stability and regulatory adherence. This involves ensuring accuracy, completeness, and monitoring of elements of the research study, such as financial transactions and billing practices. Maintaining financial activities and complying with regulations is crucial in each phase of clinical research, highlighting the importance of revenue integrity in clinical operations. Failing to comply can result in serious consequences, such as monetary fines, damage to the site's reputation, and potential legal ramifications.
Three Phases Of The Clinical Research Revenue Cycle
The clinical research revenue cycle consists of three main phases: pre-award, post-award, and closeout.
Pre-Award
The pre-award phase begins with financial management for a study, involving essential tasks such as performing Medicare coverage analysis (MCA), budgeting, and contracting. MCA helps determine billable items and services for insurance coverage, while budgeting and contracting specify detailed financial information for proper fiscal management.
Post-Award
The post-award phase of a study focuses on conducting the research, with key financial activities including financial consenting, charge segregation, billing and coding, claims review and editing, sponsor invoicing, patient insurance claims processing, and accounts receivable collection. These activities are essential for accurately recording and billing research-related charges, ensuring compliance with regulations, and maintaining financial transparency.
Close-out
During the closeout phase, the focus is on reconciling financial procedures and addressing potential risks. This involves thorough data reconciliation to identify and rectify discrepancies or errors. Risks related to billing compliance, such as MCA documentation, patient tracking, coding and billing, and reconciliation, are closely monitored and resolved with due diligence.
What Is Medicare Coverage Analysis (MCA)?
MCA is utilized to evaluate items and services within a clinical research study by carefully reviewing the protocol to determine the appropriate payor for each service. This method evaluates which items can be billed to insurance or study sponsors. It is essential to assess and document time points in accordance with the protocol schedule of assessments (items and procedures) in the billing grid to ensure precise and dependable data collection. According to the Medicare Program Integrity Manual, an item or service is deemed "reasonable and necessary” when it meets the specific criteria outlined in the guidelines. Contractors shall determine if evidence exist to consider an item or service to be reasonable and necessary if the contractor determines that the service is:
- Safe and effective,
- Not experimental or investigational (exception: routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000 which meet the requirements of the Clinical Trials NCD are considered reasonable and necessary): and
- Appropriate, including the duration and frequency that is considered appropriate for the item or service, in terms of whether it is:
- Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member;
- Furnished in a setting appropriate to the patient’s medical needs and condition;
- Ordered and furnished by qualified personnel;
- One that meets, but does not exceed, the patient’s medical need; and
- At least as beneficial as an existing and available medically appropriate alternative.
Know The Rules Of NCD 310.1
In support of patient enrollment in clinical trials and the progress of medical research, the Centers for Medicare and Medicaid Services (CMS) enacted National Coverage Determination (NCD) 310.1 Clinical Trial Policy. This policy, titled "Coverage for Routine Costs in Clinical Trials," became effective on July 9, 2007, outlining the coverage of routine costs related to qualifying clinical trials. Additionally, it includes coverage for essential items and services used for diagnosing and managing complications that may arise from participation in clinical trials. It is crucial to note that all standard Medicare regulations remain applicable in these situations, ensuring comprehensive support for participants engaging in these crucial trials.
The specific criteria within NCD 310.1 highlight the importance of conventional care and monitoring for potential complications arising from drug side effects. Take, for example, the scenario where a study drug triggers changes in cardiac arrhythmic patients. In such cases, tests like EKGs are considered essential for ensuring patient safety, especially if the medication class is known to adversely affect cardiac function. It is the standard procedure to request EKGs during patient workup in these instances, with billing procedures aligning accordingly. This adherence to NCD 310.1 criteria not only ensures comprehensive patient care but also underlines the emphasis on meeting medical standards in clinical research settings. Research billing staff needs to refer to the protocol, informed consent, pharmacy manual, investigator brochure to ascertain if the study drug is linked to any potential side effects.
6 Best Practices To Mitigate Risk
Sites that rely on best practices to track and monitor their operations can effectively comply with regulations and manage risks. This empowers sites to make informed decisions and take corrective actions when necessary to maintain the financial health of their clinical research operations. All sites should consider the following:
- A comprehensive MCA is vital for identifying billable charges and ensuring accurate billing to minimize compliance risks. This also enhances budget development by improving the efficiency of budget negotiations. Staff needs to distinguish between covered services and non-covered (research-related) services for the main payors by developing MCA based on CMS guidelines. Conducting MCA can help reduce the likelihood of submitting erroneous claims, thus avoiding potential repercussions under the False Claims Act, which aims to combat fraudulent billing practices
- The principal investigator (PI) or site staff must ensure the MCA accurately reflects the IRB-approved protocol. When a PI endorses the document, he or she confirms alignment with research parameters, validates supervision, and establishes accountability in clinical research.
- Efficient research charge review process with electronic health records (EHRs) is vital. Flagging patients and linking study activities in the EHR ensures accurate charge entry and proper patient-study association. This process guarantees comprehensive documentation and correct study attribution. The visit charges are automatically routed to EHR work queues and reviewed by the research billing office staff. The team assesses each charge to determine research-related activities versus standard of care (SOC) and appends necessary modifiers (Q0 or Q1) as per CMS requirements. This approach maintains financial integrity and compliance by categorizing charges within the research billing framework.
- Implement compliance training and provide ongoing training for staff involved in operations. Regularly perform internal billing assessments and utilize them for educational purposes within the institution.
- Embrace the opportunity to learn and grow from any billing errors made in the operational processes.
- Familiarize yourself with the coverage policies to accurately process claims related to study participation.
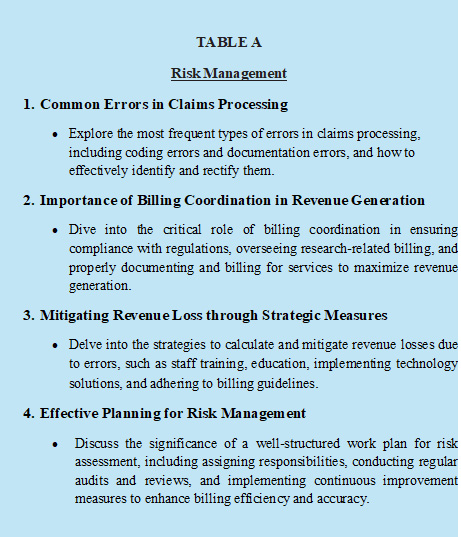
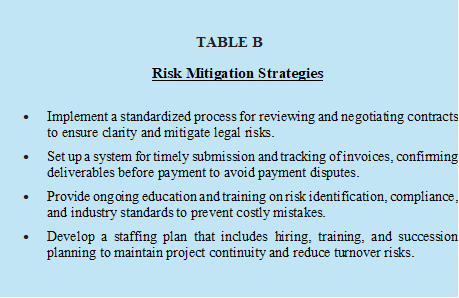
It is important to thoroughly review processes and systems in place to identify risks within a compliance framework. Risk management (Table A), reviews of past incidents, and risk mitigation (Table B) contribute to this effort.
A final word of advice is to perform an audit after enrolling around 20 patients to ensure process accuracy. Audits may be performed after enrolling only five to 10 patients, depending on study risk level. Any identified issues should be promptly fixed.
Conclusion
Upholding revenue integrity and compliance is crucial for protecting institutions and enhancing trust in the clinical research community. The activities conducted during a research study must comply with regulatory guidelines, federal rules and regulations and ethical standards. Effective communication, along with a robust framework of checks and balances and advanced technology systems, such as EHR and the CTMS, helps sites reduce risks and establish a strong clinical research billing operation. By promoting accountability and transparency, sites can safeguard their reputation and financial stability.
References:
- CMS Publication 100-08, Medicare Program Integrity Manual, Chapter 13 – Local Coverage Determinations, §13.5.4.
- Verma SK, Managing the Clinical Research Revenue Cycle to Improve the Bottom Line by Understanding Financial Strategies and Budget Negotiations. SOCRA Source Journal. 2021, Aug, issue 109
About The Author
 Dr. Sachit Verma is a board-certified healthcare leader with more than 10 years of experience in research operations, administration, revenue cycle management, and compliance within university hospitals, academic medical centers, and health systems. Leveraging his clinical research expertise, Dr. Verma has developed and executed strategies to improve pipeline development, trial delivery, and operational planning for clinical research programs. He consistently implements industry best practices, ensuring exceptional customer service delivery and effectively managing financial aspects, such as data analysis, budgeting, and various project life cycles. Additionally, Dr. Verma excels in contract management, feasibility assessments, study start-up processes, study enrollment, recruitment, ensuring participant retention, grant management, performance evaluation, and technology implementation. As an accomplished author, speaker, and board member, he merges leadership, administration, regulatory expertise, and institutional practices to ensure projects are executed within specified timelines and with successful results.
Dr. Sachit Verma is a board-certified healthcare leader with more than 10 years of experience in research operations, administration, revenue cycle management, and compliance within university hospitals, academic medical centers, and health systems. Leveraging his clinical research expertise, Dr. Verma has developed and executed strategies to improve pipeline development, trial delivery, and operational planning for clinical research programs. He consistently implements industry best practices, ensuring exceptional customer service delivery and effectively managing financial aspects, such as data analysis, budgeting, and various project life cycles. Additionally, Dr. Verma excels in contract management, feasibility assessments, study start-up processes, study enrollment, recruitment, ensuring participant retention, grant management, performance evaluation, and technology implementation. As an accomplished author, speaker, and board member, he merges leadership, administration, regulatory expertise, and institutional practices to ensure projects are executed within specified timelines and with successful results.