What Is Taking So Long For Meaningful Interoperability In Clinical Research?
By Alethea Wieland, founder and president, Clinical Research Strategies, LLC

Three decades ago when I entered the profession of clinical research, our workplace equipment extended to typewriters, white-out, mimeographs, hand-written documents, rubber erasers, pens, label makers, and fax and copy machines. Rows of massive, locked, fire-proof filing cabinets storing millions of papers for a nationally funded research program lined record rooms, hallways, and every spare corner of the offices. Most of us felt rewarded when we could use a typewriter with a correction key despite one’s typing skills being firmly judged by the illegible mistakes in the carbon copies.
Fast-forward to the present day, when countless digital technological advances, data warehouses, and hardware and software programs have made our jobs more repeatable, less erroneous, and faster. Yet, we still have not made significant progress on interoperability between disparate electronic systems such as routine, seamless, and secure data transfers from electronic health records (EHRs) to electronic data capture (EDC) systems.
The Challenge In Clinical Research — Swivel Chair Interface
Many clinical research professionals, including clinical research coordinators, clinical monitors, and clinical data managers, have complained that one of the most time-intensive and mundane manual processes in their workflow is retyping or validating information from source data existing in an EHR or a paper chart into an EDC system’s case report forms (CRFs). EDC systems are uniquely configured and validated for the maintenance and quality control of clinical trial data. The term “swivel chair interface” describes the low-level manual work performed to transfer data from one system to another. This impacts some of our most important stakeholders at the site level and remains a challenge in the industry that is taking too long to address.
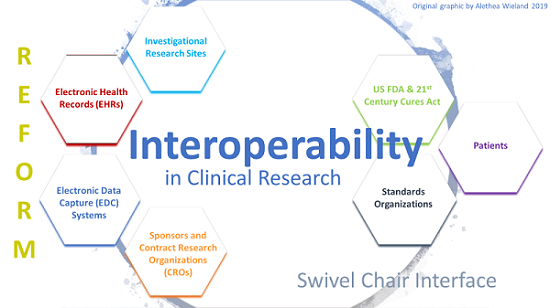
Interoperability
Interoperability, as defined by the Healthcare Information and Management Systems Society (HIMSS), “is the ability of different information systems, devices or applications to connect, in a coordinated manner, within and across organizational boundaries to access, exchange and cooperatively use data amongst stakeholders, with the goal of optimizing the health of individuals and populations.”1 Original data is moved through application programming interfaces (APIs) or third-party applications without altering the integrity of that original source once transferred or without harm to the originating system.
Much-needed reform was finally enacted into law in December 2016. The 21st Century Cures Act includes interoperability (Title III, Delivery, Subtitle A - Interoperability, Section 3001, Ensuring Interoperability of Health Information Technology) and describes the lengths at which industry must participate, conform, and adopt to advance the national agenda. The act also highlights how governmental bodies certify or decertify EHRs and guide public forums for debate and consensus for standards organizations and other impacted stakeholders.2
The Final Guidance, “Use of Electronic Health Record Data in Clinical Investigations,” issued in July 2018 by the FDA, largely points to the interoperability problem and invites industry to fix it. One of the most important changes in this guidance for sponsors and contract research organizations (CROs) is a recommendation to use EHRs certified by the Office of the National Coordinator for Health Information Technology (ONC) at the Department of Health and Human Services (HHS). For EHRs not certified by the ONC, sponsors and CROs are responsible for evaluating the EHR’s confidentiality, security, and data integrity effectiveness.3
Systems associated with clinical trial data, such as mobile applications, patient-reported outcome tools, and EDC systems, need to be controlled, maintained, and verified in conformance with 21 Code of Federal Regulations Part 11 (21 CFR Part 11), especially to satisfy the U.S. Food and Drug Administration’s inspection, recordkeeping, and retention requirements.4 EHRs do not need to be assessed for Part 11 compliance.
With such a wealth of valuable information existing in EHRs today, such as ICD-10 codes related to disease signs and symptoms, vital signs, medical history, medications, surgeries, laboratory values, radiographs, and other information derived from medical devices, in addition to the numerous ways for secure data exchange, we stand at the cusp but can’t quite cross the chasm to the next great achievement that will revolutionize clinical research.
Claims That EHRs And EDCs Are Interoperable
In response to the critical findings of the JASON Report Task Force, Final Report Oct. 14, 2014, which recommends a major shift in healthcare interoperability and health information exchange and rejects the siloed infrastructure of EHRs5, several larger EHR companies have begun to coalesce in the Argonaut Project.6 The project is privately initiated and funded to accelerate Fast Healthcare Interoperability Resources (FHIR). At the same time, select EHR companies have claimed that they have interoperable tools and standards. A recent article by Healthcare IT News managing editor Bill Siwicki describes his interviews with interoperability executives from four EHR companies — Cerner, DrChrono, eClinicalWorks, and Epic Systems – who detail the extent of their interoperability.7 What becomes most apparent from the article is that agreement on a ubiquitous definition of interoperability will not likely come any time soon.
Similarly, EDC companies have made claims of being involved with solving the interoperability problems in research, and a few pilot programs have been successful but not to the degree that has gained widespread momentum.8,9
It’s The Data Standards, Stupid
As if the U.S. healthcare system cannot become any more confusing, enter the data standards organizations and various regulatory agencies that have seats at the table. The 21st Century Cures Act legislates the imperative to establish the data standards necessary to drive adoption. The Interoperability Standards Advisory (ISA) model will be coordinated by the ONC. The ONC will spearhead “the identification, assessment, and public awareness of interoperability standards and implementation specifications that can be used by the healthcare industry to address specific interoperability needs including, but not limited to, interoperability for clinical, public health, and research purposes.” The most important takeaway is that the ISA is the authority for interfacing with the public at large and for cataloging standards and implementation specifications for all types of health IT, not just related to EHRs.10
The key standards driver is Health-Level 7 International (HL-7), the group responsible for publishing a standard for healthcare data exchange on Dec. 27, 2018, called FHIR Release 4 (R4), incorporating changes from all over the world and setting forth a normative base.11
We must also not forget the important work of the Clinical Data Interchange Standards Consortium (CDISC), whose Operational Data Model (ODM) is used throughout the international clinical research community as the gold standard, including for FDA regulatory-compliant data conformance and exchange.
And finally, on Feb. 14, 2019, the Institute for Electrical and Electronics Engineering (IEEE) published a draft set of standards to provide safe and secure interoperability for medical devices.12
Undoubtedly, there are others not included here and will be more to come.
Economic Impact Of Interoperability In Clinical Research
Reflecting on the swivel chair interface that clinical research professionals face each day, and the promise that interoperability holds for EHR and EDC systems, it stands to reason that countless manhours can be saved, including in transcription error detection. Even where half of clinical trial data is derived from EHR sources8, this translates into the following potential incalculable savings:
- Reduced costs for direct data entry paid by sponsors to investigational research sites
- Reduced on-site monitoring visits and travel expenses to perform such visits (a known revenue generator for CROs)
- Reduced menial labor associated with low morale and high turnover at investigational research sites
It takes all of us to embrace the new laws and mandates for interoperability. Putting the framework of the standards into actionable success stories will continue to take time.
References:
- HIMSS, What is Interoperability?
- 21st Century Cures Act (Title III, Delivery, Subtitle A - Interoperability, Section 3001, Ensuring Interoperability of Health Information Technology)
- FDA Guidance for Industry, “Use of Electronic Health Record Data in Clinical Investigations,” July 2018
- 21 CFR Part 11 Electronic Records; Electronic Signatures
- JASON Report Task Force, Final Report October 14, 2014
- Argonaut Project
- Siwicki, B. Epic, Cerner and others reveal just how their EHRs are interoperable, Healthcare IT News, April 5, 2019
- Conn, J. 'Swivel chair' interoperability: FDA seeks solutions to mesh EHRs and drug research record systems, Modern Healthcare, August 1, 2015
- PRWeb. New Technology Brings EHR Data to the Forefront of Clinical Research, December 4, 2017
- Interoperability Standards Advisory, The Office of the National Coordinator for Health Information Technology (ONC)
- Health-Level 7 International Fast Healthcare Interoperability Resources
- IEEE Completes Standards Family Intended to Provide Safe and Secure Medical Device Interoperability, February 14, 2019
About The Author:
 Alethea Wieland is founder and president of Clinical Research Strategies, LLC, an executive-level management consulting firm and boutique, functional service provider for the life sciences industry. Her firm’s solutions include analyzing the intersection of healthcare innovation and policy; providing flexible clinical trial resourcing; developing sustainable corporate affairs programs and policies; training and managing resilient, high-performing clinical operations teams; mitigating risks of clinical trials; and facilitating transparent, accountable sponsor-CRO partnerships. Learn more by connecting with her in LinkedIn or by visiting her website.
Alethea Wieland is founder and president of Clinical Research Strategies, LLC, an executive-level management consulting firm and boutique, functional service provider for the life sciences industry. Her firm’s solutions include analyzing the intersection of healthcare innovation and policy; providing flexible clinical trial resourcing; developing sustainable corporate affairs programs and policies; training and managing resilient, high-performing clinical operations teams; mitigating risks of clinical trials; and facilitating transparent, accountable sponsor-CRO partnerships. Learn more by connecting with her in LinkedIn or by visiting her website.
