What's In Store For EMRs After The Pandemic?
By Inga Shugalo, Itransition
In 2020, the healthcare industry went through a massive crisis caused by the COVID-19 pandemic. In some cases, the adaptation involved realizing that industry strongholds, such as care delivery models and EMR systems, needed some changes.
While providers successfully managed to introduce new models of care delivery, changing the EMR structure and logic would be too complex amidst the crisis. Now, as the pandemic has loosened its grip, the time feels right for modifying the EMR, and some statistics support the idea. Grand View Research predicts the market for EMR software development will grow further in 2021-2028. In that period, the market will be expanding at a CAGR of 3.7%.
So, what are the key points to bear in mind to make an efficient EMR system? Let’s look into the matter.
The Post-Pandemic Reality
The pandemic propelled long-awaited changes in healthcare delivery. Thus, in 2020, telemedicine consultations skyrocketed, and patients grew to trust that quality care could be achieved remotely, in the comfort of their homes. In December 2020, the U.S. Centers for Medicare & Medicaid Services (CMS) made 60 telehealth services permanent. What’s more, mHealth apps and remote patient monitoring tools also proved their reputation. They helped users reduce their exposure risks, monitor their health parameters continuously, and engage in personal health management.
As a result, the healthcare industry and its key stakeholders witnessed a meaningful shift in patients’ behavior. They transitioned from being patients to being consumers who make informed decisions, employing quality data regarding their health parameters. This is exactly where EMR systems come into play.
The New EMR Specifics
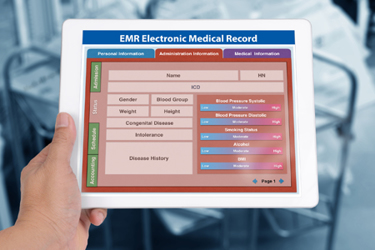
Due to the above-mentioned transformation in patients, an EMR ceased to be a doctors-only tool for adequate care provision. Hence, now an EMR system should cater to the needs and interests of two user groups — clinicians and consumers. This extended focus makes us review several EMR principles. The top ones are interoperability, data analytics for clinicians and consumers, and integration with diverse systems, including consumer health trackers.
Improved Interoperability
Interoperability, an everlasting EMR challenge, took the front stage again during the pandemic.
As we know, the most popular approaches to interoperability improvements include enabling blockchain-based EMR and secure data sharing. After the pandemic, blockchain-based EMR adoption might get some more time in the spotlight. In pre-pandemic times, the lack of interest in independent health management by patients was the key obstacle to adopting blockchain EMR systems. However, with the transition from patients to consumers and their genuine interest in self-management of their health, the situation has changed dramatically.
Today, key industry stakeholders seriously consider introducing a distributed ledger-driven EMR with global coverage. Some enthusiasts believe such a system may become a common asset for all industries connected with healthcare — pharma, labs, pharmacies, insurance, and medical researchers. Such a system may provide all users with access to complete data sets without gaps.
However inspiring the capabilities of blockchain-based EMR, providers are still cautious about the technology. They prefer to take small steps to ensure interoperability across large healthcare networks. As for the interoperability among providers, they have an opportunity to join local health information exchanges (HIEs). Such tools allow providers to share patient data across their states with no security risks. During the pandemic peak, when access to patients’ EMRs was in high demand, HIEs’ adoption also rose significantly, so such tools expanded in Nevada, Alaska, Connecticut, and other U.S. states.
Advanced Analytics
During the pandemic’s climax, analytical tools enhanced with machine learning helped clinicians assess the situation by relying on their EMRs and unstructured data. In the majority of cases, analytical tools and data sources were separate but seamlessly integrated.
However, some providers took an extra step to leverage EMR data analytics. For example, NYU Langone Health, a network of primary care providers in New York, introduced a specific population health alert into their EMR system. During the COVID-19 crisis, the alert assisted clinicians with providing adequate care and prevention for every chronic-condition patient. The alert demonstrated all gaps in care to doctors and patients in one place, thus helping both parties take timely measures to patch those gaps.
Such a progressive EMR system add-on may make a valid part of the new EMR.
Smooth Integration With Diverse Systems
An EMR system is a touchpoint that unites care teams and consumers in their pursuit of quality care and timely prevention. Therefore, such a system needs to integrate with other in-house digital systems. As for consumers, there is one more integration task involved.
As we remember, the pandemic made consumers employ their health trackers, health mobile apps, and/or devices for patient monitoring to track their health and take action when required. During the crisis, such data generated actions only when it clearly signaled some adverse event. Besides, such data may help providers and consumers reach their common goal: effective prevention.
Data should be a part of consumers’ EMRs, which calls for supporting patient-generated health data (PGHD) within the system. With such support in place, the data is automatically uploaded to the EMR. From then on, it may serve as a source of predictions regarding the likelihood of adverse health events, for both providers and consumers.
Conclusion
Amidst the pandemic, the EMR ceased to be a provider-focused tool. With the transition of patients to consumers, it is becoming equally important for them, too.
This new two-sided focus has put several EMR aspects in the spotlight for EMR developers. Thus, top features of the new EMR include streamlined interoperability, multi-source analytics, and frictionless integration with various systems. With a well-tuned EMR, consumers may act as providers’ partners, managing their health with ease and addressing potential risks timely. On the other hand, providers gain access to insightful PGHD that may help them refine population health management and prevention.
About The Author:
 Inga Shugalo is a healthcare industry analyst at Itransition, a custom software development company headquartered in Denver, Colorado. She focuses on healthcare IT, highlighting the industry challenges and technology solutions that tackle them. Inga’s articles explore diagnostic potential of healthcare IoT, opportunities of precision medicine, robotics and VR in healthcare, and more.
Inga Shugalo is a healthcare industry analyst at Itransition, a custom software development company headquartered in Denver, Colorado. She focuses on healthcare IT, highlighting the industry challenges and technology solutions that tackle them. Inga’s articles explore diagnostic potential of healthcare IoT, opportunities of precision medicine, robotics and VR in healthcare, and more.
